
During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization . For information regarding authorizations required for a member’s specific benefit plan, providers may:
. For information regarding authorizations required for a member’s specific benefit plan, providers may:
 , or
, orThese changes are announced in the form of Special Bulletins and other communications posted on Highmark’s Provider Resource Center (PRC). The most recent updates regarding prior authorization are below:
Clinical Services is phasing out fax prior authorization submissions. Providers are required to use the Availity® portal to electronically submit authorization requests, attach documentation, respond to inquiries, and check status. Click here
portal to electronically submit authorization requests, attach documentation, respond to inquiries, and check status. Click here to read last month’s article in Provider News.
to read last month’s article in Provider News.
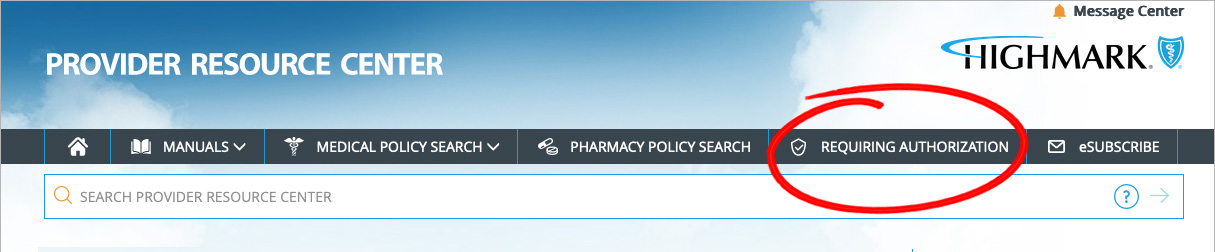
To view the full List of Procedures/DME Requiring Authorization, click REQUIRING AUTHORIZATION in the gray bar near the top of the PRC homepage.
Once redirected to the Procedures/Service Requiring Authorization page, click View the List of Procedures/DME Requiring Authorization under PRIOR AUTHORIZATION CODE LISTS.
Please note that the Highmark member must be eligible on the date of service and the service must be a covered benefit for Highmark to pay the claim.
Availity® is the preferred method for:
is the preferred method for: